News & Publications
The Milan System for Reporting Salivary Gland Cytopathology
November 29, 2018
By Liqun Yin, MD
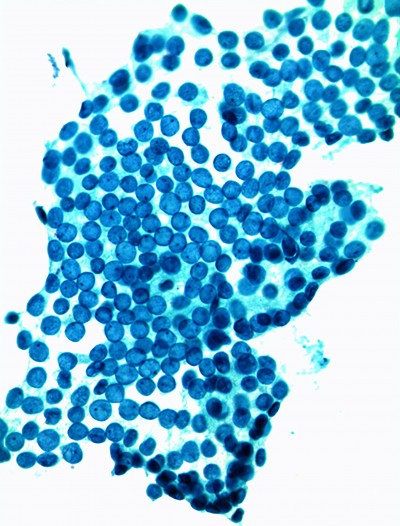
Salivary gland cytology presents many diagnostic challenges. Salivary gland tumors are one of the most heterogeneous groups of neoplasms, and salivary gland tumors are one of the most difficult areas of evaluation in cytology. The FNA sensitivity is between 86-100% with specificity somewhere between 48-94%.
The purpose of a salivary gland FNA is to provide logical clinical management and guide pre-operative strategy to the surgeon. Clear and concise results can help the surgeon prioritize and make decisions regarding what type of parotidectomy needs to be performed, and whether extracapsular dissection, superficial, subtotal or total parotidectomy is best.
There has been a general agreement on the need for a defined set of diagnostic categories, and clarity of communication regarding implicit cancer risk. Reporting can be confusing due to diverse diagnostic categories, descriptive reports without the inclusion of categories, and the use of surgical pathology terminology. This need was addressed by pathologists, molecular pathologists and ENT surgeons. The group, sponsored by the ASC and IAC, worked to devise an evidence-based, practical and user-friendly system called the Milan System of Reporting Salivary Gland Pathology.
The Milan System Includes Six Categories:
I. Non-diagnostic
- Insufficient quantitative and/or qualitative cellular material to make a cytologic diagnosis.
- Aspirate with benign elements only
- Aspirates with non-mucinous cyst contents
- Target maximum rate: 10%
- Risk of Malignancy (ROM): 10–20%
- Management: Clinical and radiologic correlation and repeat FNA
II. Non-Neoplastic
- Specimens lacking evidence of a neoplastic process: inflammatory, metaplastic, and reactive (includes acute, chronic, and granulomatous sialadenitis, sialadenosis, etc...)
- Reactive lymph nodes (flow cytometry is needed)
- Risk of Malignancy (ROM): 0–10%
- Management: Clinico-radiological correlation
III. Atypia of Undetermined Significance (AUS)
- Cannot entirely exclude a neoplasm
- Heterogeneous category, specimens are often compromised (e.g., air-drying, blood clot)
- A majority will be reactive atypia or poorly sampled neoplasms
- Target maximum rate: <10%
- Risk of Malignancy (ROM): 20%
- Management: Repeat FNA or surgery
IV. Neoplasm
IVa. Benign Neoplasm:
- Reserved for clear-cut benign neoplasms
- This category will include classic cases of PA, WT, lipoma, etc
- Risk of Malignancy (ROM): 0–7%
- Management: Conservative surgery or clinical follow-up
IVb. Salivary Gland Neoplasm of Uncertain Malignant Potential (SUMP):
- Diagnostic of a neoplasm; however, a diagnosis of a specific entity cannot be made. A malignant neoplasm cannot be excluded
- Risk of Malignancy (ROM): 20–40%
- Management: Surgery
V. Suspicious for Malignancy
- Aspirates which are highly suggestive of malignancy but not definitive
- Often high grade carcinomas with limited sampling or other limitation
- Risk of Malignancy (ROM): 60–70%
- Management: Surgery
VI. Malignancy
- Aspirates which are diagnostic of malignancy
- Sub-classify into specific types and grades of carcinoma: e.g. low grade vs high grade
- "Other" malignancies such as lymphomas, sarcomas and metastases are also included in this category and should be specifically designated
- Risk of Malignancy (ROM): 85–95%
- Management: Surgery
The Milan System
| I. Non-Diagnostic | 10–20% | Clinico-radiologic correlation & repeat FNA |
| II. Non-Neoplastic | 0–10% | Clinical follow-up & radiologic correlation |
| III. Atypia of Undetermined Significance (AUS) | 20% | Repeat FNA or surgery |
| IVa. Neoplastic: Benign | 0–7% | Conservative surgery or clinical follow up |
| IVb. Neoplastic: Uncertain Malignant Potential (SUMP) | 20–40% | Conservative surgery or clinical follow up |
| V. Suspicious for Malignancy | 60–70% | Surgery: correlate low grade vs high grade |
| VI. Malignant | 85–95% | Surgery: correlate low grade vs high grade |